| JRI | -0.23% | 13.21 | $ | |
| BCC | -1.57% | 140.35 | $ | |
| RBGPF | 100% | 61.84 | $ | |
| SCS | -0.75% | 13.27 | $ | |
| CMSC | -0.24% | 24.55 | $ | |
| NGG | 0.4% | 62.37 | $ | |
| RIO | -0.31% | 60.43 | $ | |
| CMSD | -0.02% | 24.725 | $ | |
| BCE | -1.38% | 26.84 | $ | |
| GSK | -2.09% | 34.39 | $ | |
| RELX | -0.37% | 45.95 | $ | |
| RYCEF | -4.71% | 6.79 | $ | |
| AZN | -0.38% | 65.04 | $ | |
| VOD | -0.81% | 8.68 | $ | |
| BP | 1.65% | 29.05 | $ | |
| BTI | 0.2% | 35.49 | $ |
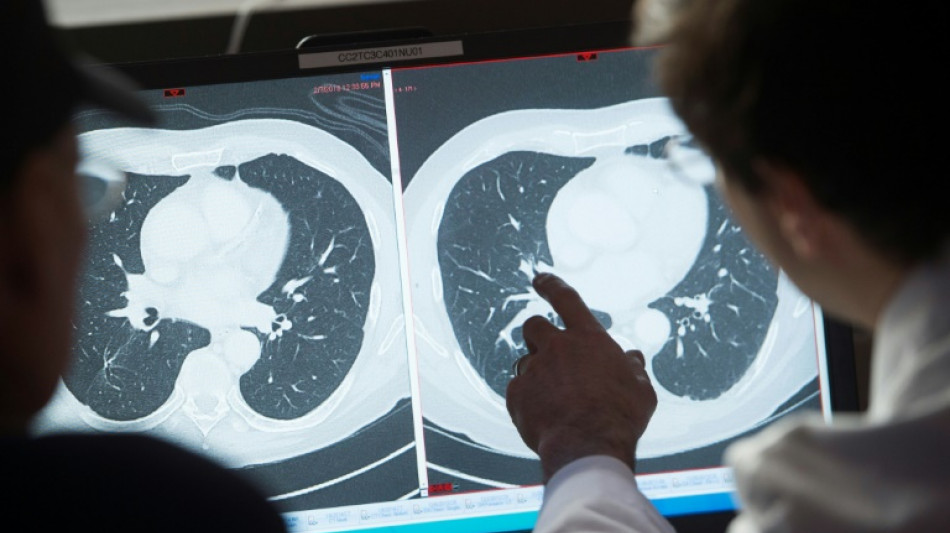
Higher cost of US cancer care doesn't improve survival rates: study
The United States spends twice as much on cancer care as the average high-income country, but gets only middle-of-the-table survival results, a study said Friday.
The results were published in the Journal of the American Health Association (JAMA) Health Forum.
"There is a common perception that the US offers the most advanced cancer care in the world," said lead author Ryan Chow, who is pursuing a medical degree and PhD at Yale University, in a statement.
America is touted for developing advanced new treatments and approving them faster than other countries, and the team were curious about whether this translated into better outcomes.
Out of 22 high-income countries, the United States was found to have by far the highest spending rate: it spends $200 billion per year on cancer care, or roughly $600 per capita, compared to the average of $300 per capita in high-income countries.
But the researchers found this additional spending did not translate into better population-level cancer mortality rates.
"In other words, countries that spend more on cancer care do not necessarily have better cancer outcomes," said Chow.
The US was only slightly better than average, while six countries -- Australia, Finland, Iceland, Japan, South Korea, and Switzerland -- had both better outcomes and lower spending.
Of the countries examined, South Korea and Japan had the lowest cancer mortality rates, while Denmark had the highest, followed by France.
Smoking is the biggest driver of cancer deaths, a factor expected to make cancer outcomes appear more favorable in countries with traditionally low smoking rates such as the US.
After controlling for smoking rates, they found the US was exactly in the middle. Nine countries -- Australia, Finland, Iceland, Japan, Korea, Luxembourg, Norway, Spain, and Switzerland — had lower smoking-adjusted cancer mortality.
There are a constellation of factors behind surging costs in the US, the team wrote.
Cancer drug expenditures account for 37 percent of privately insured US cancer expenditure, and these drugs cost far more in the US than other countries.
Unlike countries with public health systems, US state-run insurance called Medicaid cannot negotiate drug prices.
Additionally, the US Food and Drug Administration (FDA) does not consider pricing when evaluating drug approvals, unlike other countries such as Britain where cost-effectiveness must be factored.
Much of the growth in drug spending has been attributed to newer types of drugs such as monoclonal antibodies, kinase inhibitors, and immune checkpoint inhibitors, even though the evidence in their favor is often marginal.
Finally, medical care is also more aggressive in the US: "Within the last six months of life, US patients with cancer are admitted to the intensive care unit at twice the rate of other countries and are more likely to receive chemotherapy," the team wrote.
Specialty societies advocate for more screening than guidelines suggest, further increasing costs, and low-risk tumors, such as early-stage prostate cancers, are more often subject to intervention despite evidence they would unlikely cause harm if untreated.
"Other countries and systems have much to teach the US if we could be open to change," said co-author Elizabeth Bradley, president of Vassar College.
T. Jones--BTZ
 London
London

 Manchester
Manchester
 Glasgow
Glasgow
 Dublin
Dublin
 Belfast
Belfast
 Washington
Washington
 Denver
Denver
 Atlanta
Atlanta
 Dallas
Dallas
 Houston Texas
Houston Texas
 New Orleans
New Orleans
 El Paso
El Paso
 Phoenix
Phoenix
 Los Angeles
Los Angeles



